HEDIS/Hybrid Season is Upon Us!
Let’s have a conversation
The Healthcare Effectiveness Data and Information Set (HEDIS), a set of performance indicators, is required by the Centers for Medicare and Medicaid Services (CMS) for all Medicare Advantage plans. It is a tool utilized to monitor outcomes related to clinical quality and preventative care across health plans and has significant impact on Medicare Stars. HEDIS data can be calculated either utilizing administrative data within the claim or encounter, supplemental data, or hybrid data review. Hybrid data requires additional information through medical record review to provide the full picture of the care provided. HEDIS season is the last opportunity to focus on HEDIS measure improvement efforts for Star Year 2023.
Maximizing your Chart Retrieval Process for HEDIS
Performing a review and analysis of the medical records is critical to the success of HEDIS/Hybrid season and maximizing abstraction efforts. Medical record outreach to providers can be completed in multiple ways, such as fax, mail, on-site collection, electronic medical record (EMR) access, etc. From HEDIS pre-planning efforts to the pull of the initial rates, health plans need to be focused and have strategies in place for early and often outreach.
Below we discuss three key themes outlining a successful HEDIS/Hybrid strategy.
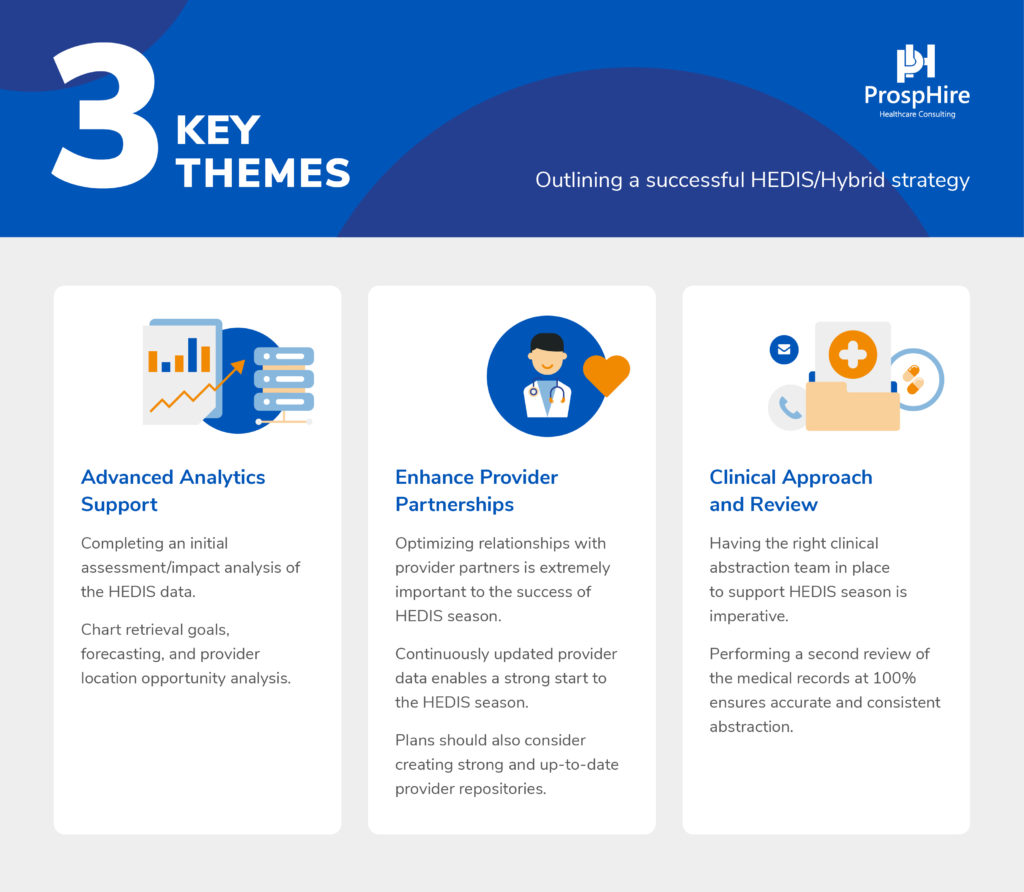
Advanced Analytics Support
- Completing an initial assessment/impact analysis of the HEDIS data as your initial rates/sample is pulled gives your team a great perspective on the season ahead and allows for strategy development. This enables your team to have a clear understanding of opportunities and strategies to pursue throughout the season.
- Plans are encouraged to have reporting to allow leadership insight into performance as the season progresses. This includes chart retrieval goals, forecasting and provider location opportunity analysis, which allows for better communication and more informed decision-making.
Enhance Provider Partnerships
- Optimizing relationships with provider partners is extremely important to the success of HEDIS season. Plans typically have internal communications, tools, trainings and resources available to better assist provider partnership.
- Continuously updated provider data enables a strong start to the HEDIS season and in turn will help reduce provider abrasion and ensure your requests are ‘first in the door’ with providers.
- Plans should also consider creating strong and up-to-date provider repositories. This repository/database will go a long way to help ensure the information is passed from season to season such as a list of providers that require on-site retrieval or providers with EMR access.
Clinical Approach and Review
- Having the right clinical abstraction team in place to support HEDIS season is imperative. Ensuring the team is established in prior to the new year, allows for trainings and educations to be completed ahead of the start of the season. This clinical abstraction team will make the clinical connections that can improve HEDIS outcomes.
- Performing a second review (over-read) of the medical records at 100% ensures accurate and consistent abstraction with every medical record retrieved.
At ProspHire, we continue to partner with Health Plans, to offer insights, analysis and execution strategies to improve Star ratings. Do you need support to optimize your HEDIS season? Let's have a conversation.
ProspHire
216 Blvd of the Allies, Sixth Floor
Pittsburgh, PA 15222
412.391.1100
[email protected]


© 2024 ProspHire, LLC. All Rights Reserved / Terms of Use / Privacy Policy