Scaling or Optimizing Your Medicaid Operations in Nevada? We’ve Got You Covered
Let’s have a conversation
There is a saying in the Medicaid community of “if you know Medicaid in one state, you know Medicaid in one state” given the variation in program eligibility, services and operations across states. While this remains true, there are fundamentals in Medicaid services, quality performance and operations that remain the same nationally.
As health plans seek to differentiate themselves in the market and deliver a member-first program, ProspHire supports health plans in establishing a strategic roadmap that integrates organizational goals and unique regional membership needs. ProspHire is dedicated to a regional approach to product development, quality programs, and member engagement. Demonstrating this commitment, ProspHire leverages and promotes the use of social determinant of health and other publicly available data sources to develop data-driven strategies and identify key steppingstones to appropriately address unique health plan membership needs. Check out our data dashboard!
Medicaid plans seeking to outperform will need to look beyond their bottom line and focus on the successful delivery of care and resulting outcomes for their membership. ProspHire collaborates with health plans to bring vision and strategy to execution and reality as a partner to your organization and your community.
The recent announcement of the intent to award Medicaid contracts in Nevada presents both opportunities and challenges for health plans. Whether you are an incumbent plan seeking to optimize performance or a new entrant preparing for go-live, ProspHire specializes in providing strategic support to drive operational success.
Opportunities in Focus
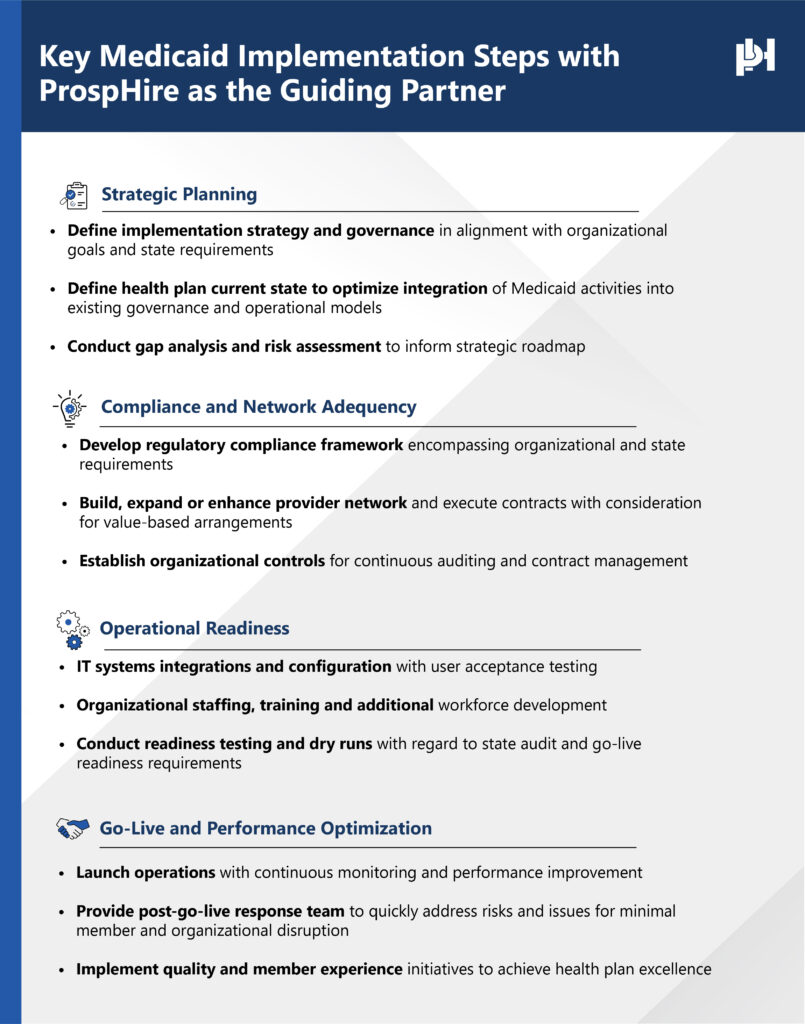
- Operational Readiness
- Develop and execute a comprehensive implementation plan to meet state requirements. Establish effective workflows, IT system integration and operational policies.
- Conduct readiness assessments to mitigate risks prior to go-live.
- Provider Network Expansion & Management
- Assess and expand provider networks to meet state adequacy standards.Implement contracting strategies to enhance access to care and quality measure performance.
- Improve provider relations and streamline credentialing processes.
- Regulatory Compliance
- Ensure alignment with Nevada Medicaid regulations and reporting requirements. Conduct compliance audits and gap analyses.
- Develop policies and procedures to maintain ongoing compliance.
- Quality Programs, Performance & Addressing Health Disparities
- Optimize HEDIS and Medicaid quality measures to improve performance. Implement care management programs to enhance member health outcomes. Align quality initiatives with state and federal benchmarks.Implement social determinants of health (SDOH) strategies. Develop community engagement initiatives to improve equity in care.
- Leverage data analytics to identify and address disparities.
- Member Experience
- Improve CAHPS and member satisfaction scores through targeted interventions.
- Develop data-driven member engagement strategies.
- Administrative Cost Savings
- Identify cost-containment opportunities to maximize efficiency. Streamline operations to reduce administrative burden through systems integration, process automation and strategic workflow optimization.
- Leverage technology to enhance claims processing, contracting and other productive repetitive activities.
ProspHire Can Help
By partnering with us, health plans can confidently navigate the complexities of Medicaid implementation and achieve operational excellence in Nevada’s evolving landscape. Contact us today to learn more about how we can support your success.
ProspHire
216 Blvd of the Allies, Sixth Floor
Pittsburgh, PA 15222
412.391.1100
prosper@prosphire.com


© 2025 ProspHire, LLC. All Rights Reserved / Terms of Use / Privacy Policy