How Dental Practices Can Achieve Workflow Optimization
Effective communication keeps dental practice workflows running smoothly, from the front desk to the operatories and waiting rooms. Communicating and sharing data across teams and devices allows practitioners to provide empathetic and optimized patient experiences.
Dental practices have various options for digitizing and optimizing equipment. Achieving dental practice workflow optimization through design thinking and emerging technology will boost productivity and enhance the overall quality of patient care. Let’s explore dental practice management and strategies for improving front and back-office workflows.
Understanding Dental Practice Workflow
A dental practice must consistently deliver excellent oral healthcare services to patients. An efficient workflow organizes and streamlines these processes, allowing for a smooth patient stream, shorter wait times and effective coordination among staff.
Dental practice workflows include tasks such as:
- Scheduling appointments
- Checking-in patients
- Collecting medical history
- Performing examinations and treatments
- Facilitating proper follow-up care
- Managing insurance and patient collections
A well-designed dental practice workflow addresses potential bottlenecks, reducing errors and improving communication. The three areas that often experience slowdowns are the reception areas, sterilization rooms and operatories. Paperwork, non-digital impressions and inaccessible online information throughout the dental practice are the primary culprits.
Here are other obstruction causes.
- Schedule Utilization: Overbooking and downtime could mean your scheduling needs improving.
- Time management: Dental practices need to account for the time it takes to discuss treatments and insurance with patients on top of the time required to diagnose, anesthetize or treat. . A lack of time management can increase patient wait times and general practice availability.
- Practice resourcing: Dental practitioners and staff are in high demand. Many offices struggle to properly staff their practices on a regular basis, which creates challenges efficiently managing full schedules.
While bottlenecks can occur anywhere and anytime, regardless of planning, digital workflow optimization strategies can streamline and automate some processes, opening more opportunities for your practice.
The Importance of Design Thinking and Emerging Technology in Dental Practices
Workflow optimization involves improving effectiveness. The goal is to create a more efficient environment, allowing dental professionals to provide high-quality, timely care while ensuring a positive patient experience. Streamlining processes may include coordinating tasks better among dental staff, but it often involves implementing emerging technologies and digital systems with design thinking.
Design thinking is a creative problem-solving approach focused on understanding people’s needs and finding practical solutions, which are especially applicable to those providing patient-centered healthcare services. It involves compassion, experimentation and collaboration to develop innovative solutions to various workflow challenges.
Technology use has increased among healthcare providers and dental practices worldwide. In 1984, only 11% of dental practices in the United States used computers. Today, teledentistry is equally as effective as in-person consultations for diagnoses and assessments.
Here are other time-saving technology examples that have improved dental practice workflow.
- Digital radiography: Digital X-ray systems instantly produce high-quality images for diagnostic purposes, allowing dental professionals to save, send and view the images from nearly any device.
- Electronic health records: Digital patient record management systems streamline documentation and give different healthcare providers easy access to patient information when needed.
- Intraoral cameras: Small handheld cameras capture detailed images of patients’ oral cavities and dentition, aiding in diagnosis and treatment planning without sending dental impressions to a lab.
- CAD/CAM technology: Computer-aided design and computer-aided manufacturing systems allow you to create same-day dental restorations like crowns and veneers, eliminating the need for multiple appointments and temporary fixes.
- Communication tools: Secure messaging and teleconferencing platforms allow efficient communication among dental team members, specialists and patients.
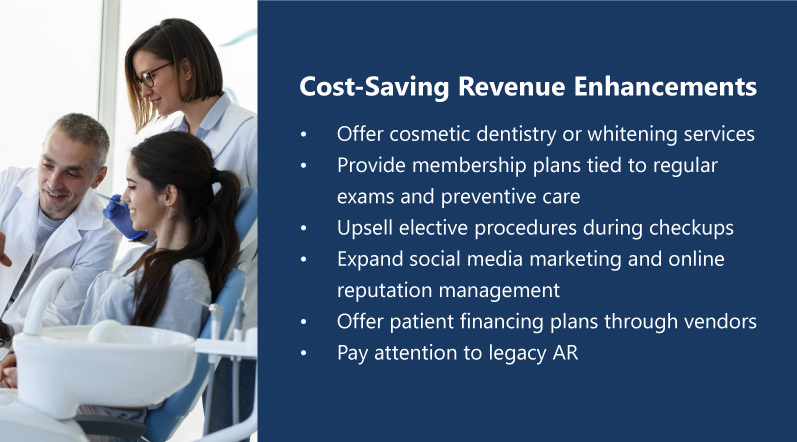
- Management software: Dental practice management software helps with appointment scheduling, billing, inventory management, patient communication and overall organization. The ideal solution is to have one platform that can handle everything in the same place without switching between different devices or programs.
- Automated appointment reminders: Some tools can automatically send reminders to patients via text messages or email, reducing no-shows and optimizing appointment scheduling.
How to Use Design Thinking and Emerging Technology in Your Dental Practice
Using manual processes will limit your productivity, overwhelm your team and prevent you from having a competitive edge. To achieve workflow optimization with emerging technology, you can introduce new software and processes by following these steps.
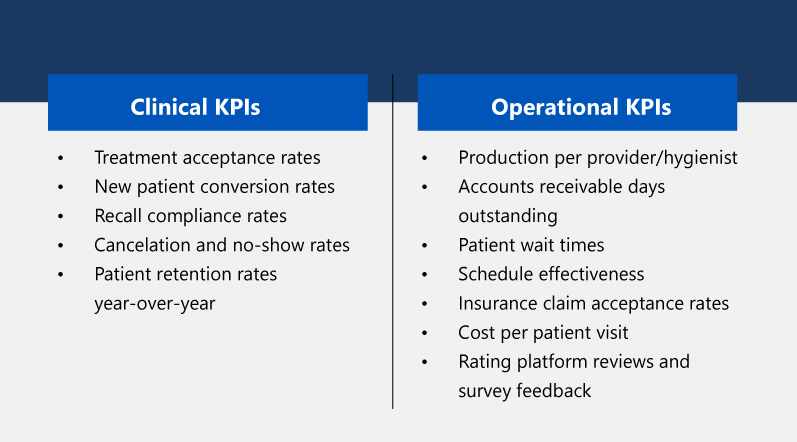
- Identify workflow challenges: Start by analyzing your existing workflows and finding areas for improvement. This step may involve studying your patients’ experience, appointment booking system, treatment planning and revenue cycle management.
- Involve your dental team: Gather your team’s input and insights regarding their workflow challenges. Their firsthand experience and expertise can provide valuable insights into areas that require optimization and improvement.
- Map your current workflow: Create a visual representation of the existing workflow to understand the sequence of steps, handoffs between team members and the potential bottlenecks.
- Identify opportunities for improvement: Analyze your mapped workflow to identify where you can enhance your efficiency, eliminate redundancies and automate manual tasks. Look for opportunities to standardize processes, reduce paperwork and leverage technology solutions to streamline your operations.
- Find solutions to implement: Effect technology that can automate tasks, improve communication and centralize all your information.
- Redesign your workflow: Remodel the workflow based on the areas of improvement and technology solutions you found. Determine the best task sequence and handoffs between team members and incorporate tech that will enhance these tasks’ efficiency.
- Implement and test: Apply the redesigned workflow in phases, starting with specific processes or a pilot group. Train your team to ensure they are comfortable with the changes.
- Continuous evaluation and improvement: Monitor and evaluate the effectiveness of the new workflow and gather feedback from the team. Identify any issues or areas that require further refinement and make necessary adjustments.
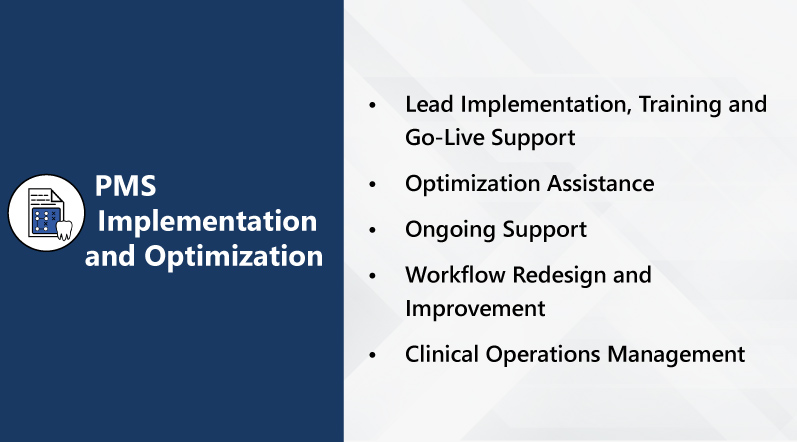
Optimize Your Dental Practice with ProspHire
Workflow optimization is a continuous process. Thus, you should always seek ways to improve and adapt to meet changing needs. It requires a strategic approach that combines design thinking principles with emerging technology. When you partner with ProspHire, we work with you and your dental team to identify challenges and opportunities to create a more efficient, patient-centered and productive environment.
To learn more about our dental practice management services, contact us by filling out our online form or giving us a call.