State SNP Alignment: Impacts and Opportunities for Health Plans
Let’s have a conversation
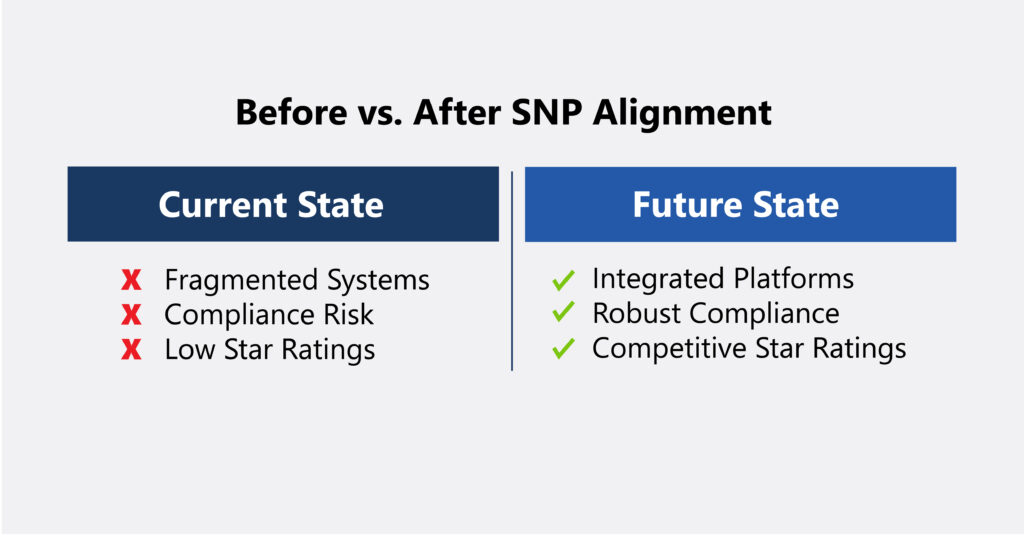
In the 2025 Medicare Advantage and Part D Final Rule, CMS introduced several enrollment updates for Dual Eligible Special Needs Plans (D-SNPs) aimed at improving the integration of Medicare and Medicaid services for individuals fully eligible for both programs. The rule provides guidelines that state, starting in 2027, D-SNPs must adopt exclusively aligned enrollment when paired with an affiliated Medicaid plan.
Additionally, in the Proposed Final Rule for CY2026, CMS reinforces its stance on enhancing the experience of dual eligible members. Proposed provisions include requirements to create a more seamless and integrated experience, such as implementing an integrated member ID card and streamlining the health risk assessment (HRA) and individualized care plan (ICP) processes.
As CMS and state governing agencies move toward aligning D-SNPs with Medicaid programs, health plans will face operational, enrollment, quality and member experience headwinds.
To successfully implement these changes, health plans must evaluate the impact on the key areas outlined below and develop strategies to execute them seamlessly, prioritizing member experience and delivering value.
Key Impacts of D-SNP Alignment
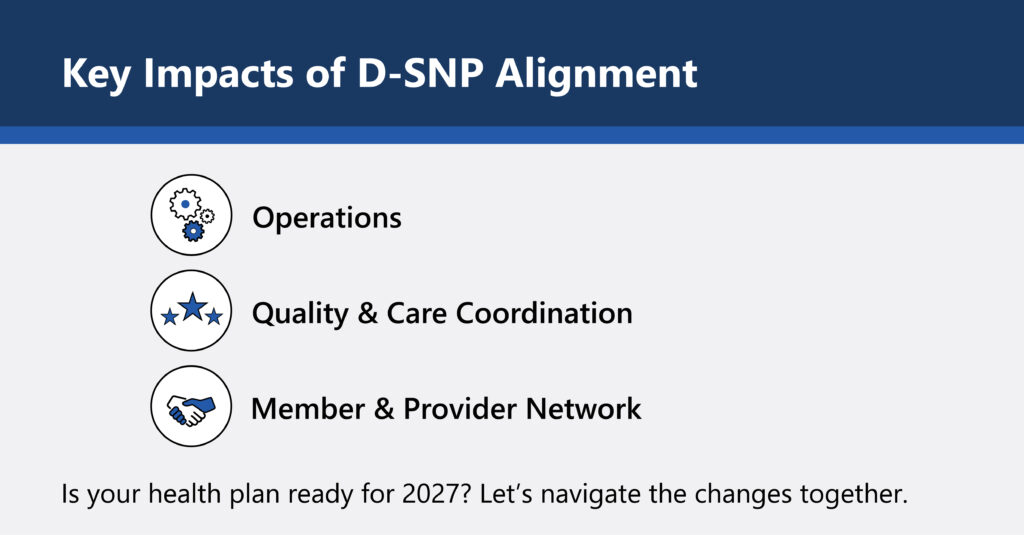
Operations
- Unifying Medicare Advantage and Medicaid systems for seamless care coordination
- Keeping up with complex and evolving state and federal regulations
- Preventing membership losses during auto-enrollment transitions
Quality & Care Coordination
- Ensuring integrated care coordination improves efficiency and outcomes
- Balancing comprehensive performance on Star Ratings, HEDIS measures, and relevant State quality programs
- Addressing SDOH to meet state requirements and improve member outcomes
Member & Provider Network
- Educating providers on new claims, payment and care coordination processes
- Simplifying dual-eligible member experiences to reduce confusion
- Maintaining continuity of care during transitions to aligned plans
Is your health plan ready for 2027? Let’s navigate the changes together.
Impact on Health Plan Operations
Identifying impact on the key areas below is necessary to ensure plans can meet D-SNP alignment requirements, including:
- Systems Integration: Plans must integrate Medicare Advantage and Medicaid platforms to allow for data sharing and effective care coordination and care management
- State and Federal Regulatory Compliance: The increase of state and federal regulations will require more oversight and monitoring to ensure compliancy
- Enrollment Processes: Dual-eligible individuals may experience a smoother enrollment process into aligned plans, potentially boosting membership in dual-eligible SNPs
- Member Retention: Alignment guidelines may result in members being auto enrolled into specific plans, which could lead to membership losses during the process if members are moved to a competitor’s plan
Impact on Health Plan Quality and Care Coordination
Aligned SNPs present opportunities and challenges to quality improvement:
- Improved Care Coordination: Improved integration between Medicare and Medicaid services is expected to enhance quality by streamlining processes for member engagement, completing health risk assessments and coordinating care
- Focus on Star Ratings and HEDIS Measures: Both Medicare Star Ratings and Medicaid quality measures will need to remain competitive and plans will need to prioritize performance
- Social Determinants of Health (SDOH): SNP alignment highlights the importance of addressing SDOH to improve member outcomes and meet state contract expectations
- Continuity of Care: Through integrated networks, plans aligned across state Medicaid programs may offer better continuity of care and may experience minimal to no disruption
Impact on Health Plan Members and the Provider Network
For members, the shift to aligned SNPs can improve care experiences but also introduces complexities that could lead to provider and member confusion and abrasion if not changes are not executed thoroughly:
- Provider Education: Plans will need to educate providers on changes for dual-eligible members for areas such as claims submission and payment, benefit design and care coordination
- Simplified Benefits: Members may benefit from the increased between Medicare and Medicaid benefits enabling a streamlined approach to accessing care
- Continuity of Care: Plans aligned across state Medicaid programs may offer better continuity of care through integrated networks.
How ProspHire Simplifies D-SNP Alignment
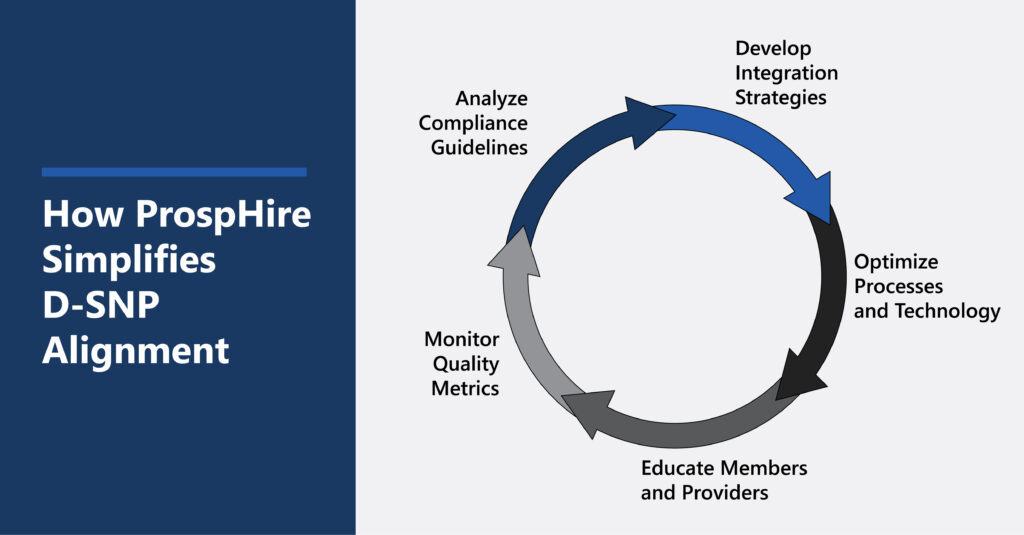
- Analyze Compliance Guidelines
- Develop Integration Strategies
- Optimize Processes and Technology
- Educate Members and Providers
- Monitor Quality Metrics
How ProspHire Can Help
At ProspHire, we support health plans through navigating complex transitions like D-SNP alignment requirements. Our deep expertise in healthcare strategy, operations and compliance, ProspHire is here to support plans by:
- Analyzing compliance guidelines to fully understand regulatory requirements
- Developing strategies for seamless Medicare-Medicaid integration across cross-functional business areas
- Supporting operational readiness through technology, process optimization and member and provider educational opportunities
- Identifying quality improvement opportunities tied to dual-eligible populations
By partnering with ProspHire, health plans can navigate the complexities of SNP alignment confidently, ensuring sustainable growth and improved outcomes for dual-eligible members.
Schedule Your SNP Alignment Consultation Today!
© 2025 ProspHire, LLC. All Rights Reserved / Terms of Use / Privacy Policy






